- Visibility 194 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijirm.2024.021
-
CrossMark
- Citation
Expert perspectives on the use of antihistamines in managing allergic rhinitis in Indian settings: A cross-sectional study
Introduction
Allergic rhinitis (AR) is the most common atopic condition, affecting approximately 10% to 30% of adults and up to 40% of children worldwide. It causes symptoms such as nasal congestion, clear runny nose, sneezing, postnasal dripping, and nasal itching, causing significant discomfort for affected individuals and societal impacts.[1], [2] Despite being perceived as a minor health issue, AR can significantly affect an individual's quality of life.[3] Studies indicate a concerning rise in AR cases over the years. The International Study of Asthma and Allergies in Childhood (ISSAC) Phase 1 (1998) and Phase 3 (2009) both highlight an escalation in nasal symptoms and allergic rhinoconjunctivitis among children aged 6-14.[4]
The global prevalence of AR among adults varies between 18% to 40%, whereas in India, approximately 20% to 30% of individuals were affected by this condition. In India, AR affects around 30% of the population. It has been observed that 15% of those suffering from AR eventually develop asthma.[5] Studies indicate that AR symptoms affect approximately 75% of children and 80% of adults with asthma in India.[6], [7] Similarly, a recent study by Sanjay et al. in Mysore reported a consistent increase in AR cases over 15 years (1998-2013) in pediatric group.[8]
Antihistamines are established as the primary treatment for AR, effectively alleviating symptoms by blocking histamine receptors on nerve cells. They can be used alone or in combination therapy to achieve comprehensive symptom relief, especially in mild to severe cases. An observational study in Asia found that over 50% of patients with AR were primarily treated with antihistamines, followed by approximately 30% using nasal spray steroids.[9], [10] The biological effects of histamine in allergic reactions are mediated through H1 receptors, which exist in both active and inactive forms of G-protein-coupled receptors that balance each other.[11] The first- generation antihistamines were found to have sedative properties, which were considered a major drawback. To address these limitations, subsequent modifications were implemented during the development of second-generation antihistamines. Notably, major guidelines from organizations such as the American Academy of Allergy, Asthma & Immunology (AAAAI), the American College of Allergy, Asthma & Immunology (ACAAI), and the European Academy of Allergy and Clinical Immunology (EAACI) recommend the use of second-generation antihistamines as the first-line treatment for allergic rhinitis (AR). This recommendation is based on their proven effectiveness and lower risk of sedative side effects compared to first-generation antihistamines.[12], [13]
Bilastine, a second-generation antihistamine acting on the H1 receptor, stands out as a novel, safe, and well-tolerated option for treating AR symptoms. Its recent approval underscores its efficacy in managing AR symptoms. The extended duration of action, effectiveness, minimal sedation, and low-performance impairment of bilastine distinguish it from other second-generation antihistamines.[11], [14] Antihistamines as a standalone therapy may not comprehensively alleviate all AR symptoms. Therefore, they are often combined with leukotriene receptor antagonists like montelukast, which inhibit leukotriene production, to achieve more comprehensive symptom management.[15], [16] Montelukast, a leukotriene receptor antagonist, acts orally to selectively block the action of leukotrienes on their receptors. By specifically targeting cysteinyl leukotrienes D4 (LTD4) at the cysteinyl leukotriene receptor, it effectively prevents airway edema and smooth muscle contraction. Consequently, this action reduces the secretion of thick and viscous mucus, alleviating AR symptoms.[15] When combined with antihistamines, montelukast can offer a comprehensive reduction in both daytime and nighttime AR symptoms. The synergistic effect of these medications addresses multiple pathways involved in allergic responses, providing enhanced relief for individuals suffering from AR.[17]
Understanding the prescription practice of antihistamines in Indian settings may help improve patient management and develop consensus to optimize the treatment for AR. The present survey-based study aims to gather clinicians' perspectives regarding the use of antihistamines for the management of AR in Indian settings.
Materials and Methods
We carried out a cross-sectional study among clinicians in managing AR in the major Indian cities from June 2023 to December 2023. The study was conducted after receiving approval from Bangalore Ethics, an Independent Ethics Committee which was recognized by the Indian Regulatory Authority, Drug Controller General of India.
An invitation was sent to leading specialists in managing AR patients in the month of March 2023 for participation in this Indian survey. About 180 experts from major cities of all Indian states representing the geographical distribution shared their willingness to participate and provide necessary data. The questionnaire booklet titled ABLE (Allergic Rhinitis with Asthma Management: Role of Bilastine + Montelukast combination) study was sent to the physicians who were interested to participate. The ABLE study questionnaire consisted of 26 questions addressing current feedback, clinical observations, and the clinical experience of specialists in managing AR using antihistamines in routine settings. Clinicians had the option to skip any questions they preferred not to answer. They were instructed to complete the survey independently, without consulting their colleagues. Written informed consent was obtained from all participants before the study commenced.
Statistical analysis
The data were analyzed using descriptive statistics. Categorical variables were presented as percentages to provide a clear insight into their distribution. The frequency of occurrence and the corresponding percentage were used to represent the distribution of each variable. To visualize the distribution of the categorical variables, graphs, and pie charts were created using Microsoft Excel 2013 (version 16.0.13901.20400).
Results
The survey consisted of 180 clinicians, of whom 34% reported that approximately 20% to 30% of patients presenting to the outpatient clinics have allergic rhinitis (AR), while 33% responded that 30% to 40% have AR. AR is commonly seen in patients aged between 35 to 45 years as reported by 29 % of the clinicians. About 48% and 45% of the clinicians reported nasal congestion as the common and bothersome symptom for AR, respectively. Approximately 52% of clinicians reported blocker as the most common type of AR encountered by patients, while 48% of them opined sneezer as the common type of AR.
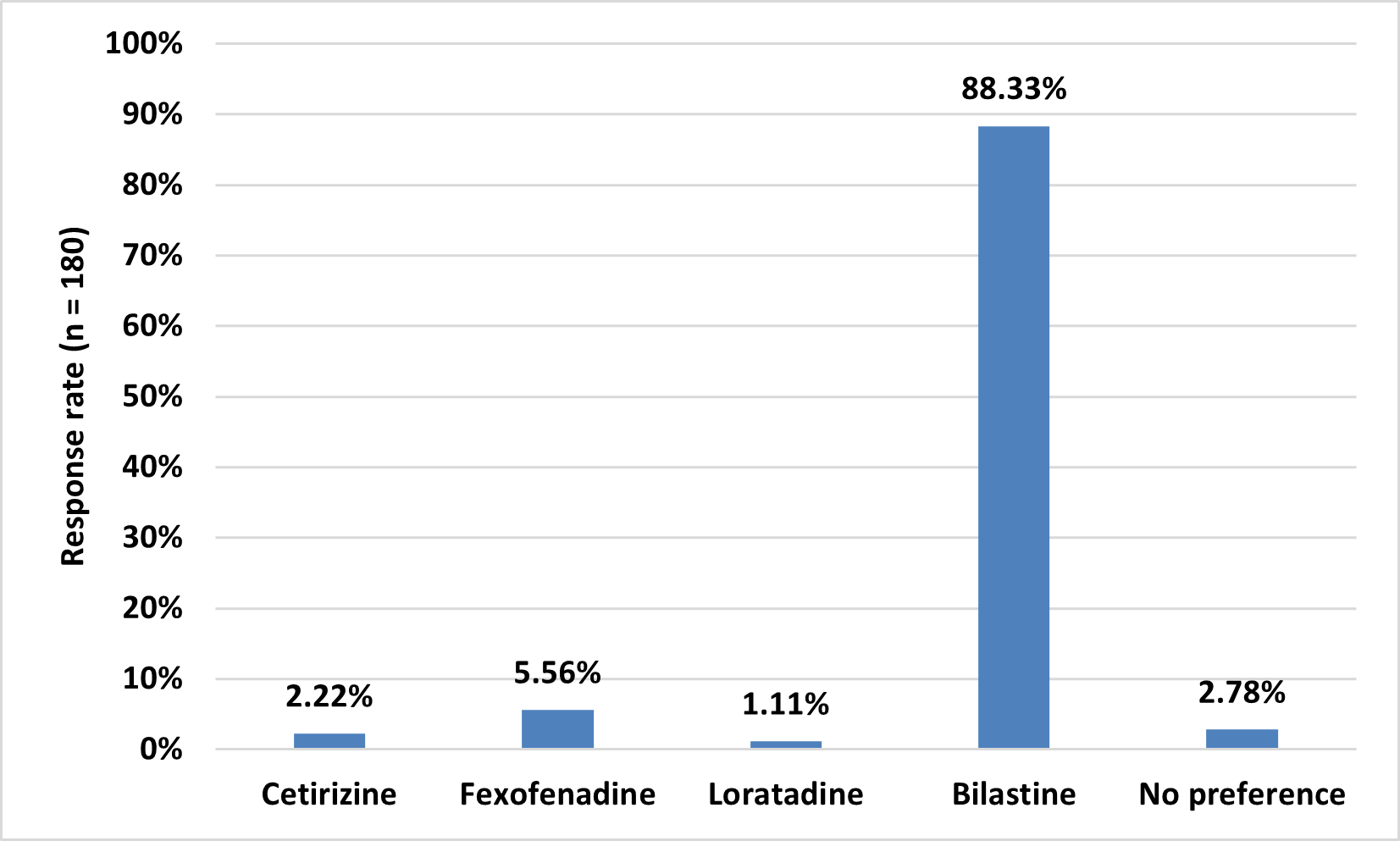
About 45% of the clinicians reported that clinical history is significant for confirming the diagnosis of AR. More than half (56.67%) of the clinicians reported bronchial asthma as a common co-morbidity encountered while treating patients with AR. Around 30% to 40% of patients with AR experience significant impairment in their quality of life. Majority (61.67%) of the clinicians reported that they do not perform skin prick allergy tests. According to 39% of the clinicians, more than 40% of the respondents seek non-sedating antihistamine tablets. Majority (88.33%) of the clinicians reported bilastine as the preferred choice of antihistamine for treating patients with AR ([Figure 1]).
About 39% of the clinicians responded that 4 weeks was the typical duration of treatment for patients with moderate to severe AR. According to 62% of the respondents, non-sedating action was an important factor to be considered when choosing an antihistamine medication for a patient with AR ([Table 1]).
|
Factors |
Response rate (n = 180) |
|
Non-sedating action |
62.22% |
|
Severity of the allergy |
26.11% |
|
Other medical conditions such as renal/altered liver function/cardiac condition |
8.33% |
|
Presence of co-morbid allergic conditions |
3.33% |
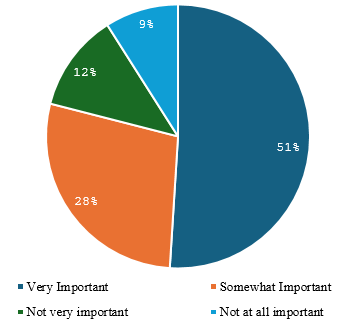
About 44% of clinicians preferred prescribing intranasal corticosteroid nasal spray to approximately 20% to 30% of their patients and 31% reported prescribing it for a one-month course. Half of the clinicians (50.56%) opined that considering the cost of treatment when managing patients with AR was very important ([Figure 2]).
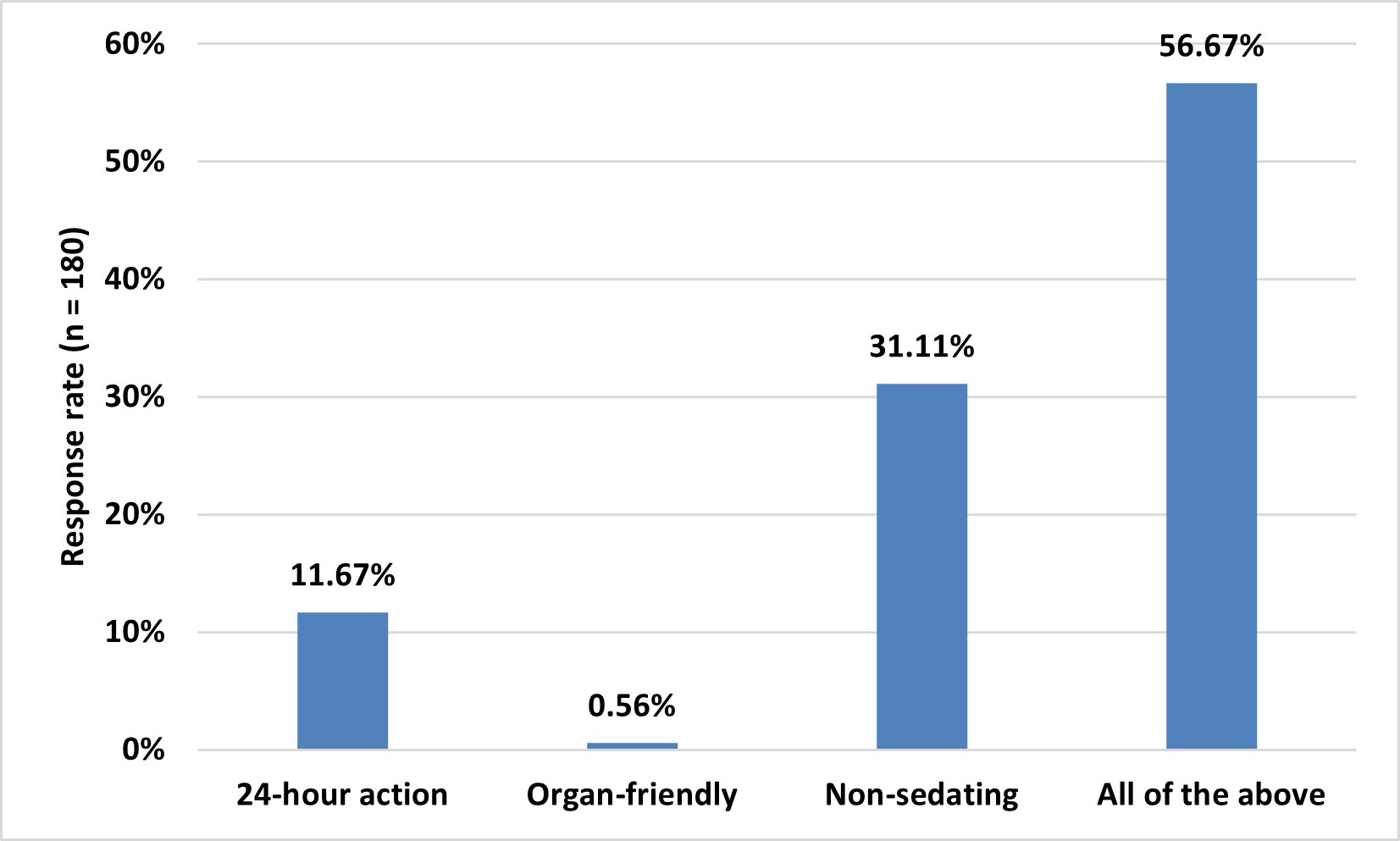
Most of the clinicians (86.67%) reported that they utilize a standardized questionnaire to gather patient history information. Majority (86.11%) of the clinicians opined that they and their staff allocate additional time to educate patients on environmental control measures and allergen avoidance strategies. About 86% of clinicians agreed that they demonstrate nasal irrigation or spray administration to patients. Around 79% of clinicians stated that they believe specialized training in allergy is necessary for better management of patients with AR. The primary advantages of bilastine, reported by 57% of clinicians ([Figure 3]), were its non-sedating nature, organ-friendly profile, and rapid action within 24 hours.
As reported by 47% of clinicians, 10-25% of patients with AR have concomitant bronchial asthma. Approximately 63% of respondents stated that antihistamines combined with montelukast were the preferred treatment for patients with persistent AR ([Table 2]). Around 57% of clinicians reported that antihistamine therapy was beneficial in cases with upper respiratory tract infections. About 43% of clinicians opined that review articles on the latest research and treatment guidelines were the type of resources on AR that would be most useful to healthcare professionals. Almost 67% of respondents reported that when educating patients with AR, patient education leaflets were typically used to provide information.
|
Treatment |
Response rate (n = 180) |
|
Antihistamines + montelukast |
63.33% |
|
Antihistamines + montelukast + topical corticosteroids |
27.78% |
|
Antihistamines or montelukast with topical corticosteroids |
4.44% |
|
Antihistamines |
4.44% |
Discussion
The survey findings advocate for evidence-based approaches and resource utilization, including review articles and patient education leaflets, to enhance healthcare delivery and patient outcomes in AR. The study also emphasizes the impact of AR on quality of life, indicating a preference for bilastine and combination therapy with montelukast for effective disease management.
Majority of the clinicians preferred bilastine as the preferred antihistamine for treating AR. This preference was supported by several previous study findings. Bousquet et al. reported that bilastine is safe and well-tolerated even after 1 year of treatment, recommending it as one of the preferred prescriptions for AR treatment.[18] Randhawa et al., in a meta-analysis based on moderate to high-quality evidence, concluded that bilastine was effective and safe in treating overall AR symptoms with comparable efficacy and safety.[19] In a PAN-India survey study, Bhagat et al. found that most physicians prefer bilastine as an antihistamine due to its low sedative potential and high effectiveness. Bilastine was also the preferred treatment option for patients with mild to moderate hepatic or renal impairment, as well as those suffering from persistent AR.[20]
The current study emphasized that non-sedating action was a critical factor to be considered when choosing an antihistamine medication for a patient with AR. The sedative effects associated with antihistamines can limit their efficacy, primarily due to their inhibition of central histaminergic neurons in the brain. In the current survey, bilastine was highlighted as one of the least sedative antihistamines, making it a preferred choice in AR treatment. Studies have consistently shown that second-generation antihistamines, characterized by their low sedation potential, were widely used in children for managing AR. This preference was based on their safety profile and reduced risk of sedative side effects compared to first-generation antihistamines. The non-sedating nature of these medications was particularly advantageous for pediatric patients, allowing effective symptom relief without significant impairment of cognitive function or daytime drowsiness.[10], [21], [22]
AR impacts both children and adults, imposing significant costs related to disease management and lost productivity due to illness-related work absences. Management strategies for AR include allergen avoidance, pharmacotherapy, and allergen immunotherapy, with evaluation of cost-effectiveness being crucial for optimal disease control.[23] Bousquet et al. also highlighted the substantial cost associated with persistent AR, underscoring the economic burden of this condition.[24] Singh and Kumar concluded that there was considerable variation among second-generation antihistamines, which influences the treatment approach for AR patients.[25] Aligning with previous findings, the present study emphasized the importance of considering the cost of treatment when managing patients with AR.
According to the current survey respondents, the primary advantages of bilastine were its non-sedating nature, organ-friendly profile, and rapid onset of action within 24 hours. Jáuregui J et al. reported that bilastine was rapidly absorbed, non-sedative, and undergoes no hepatic metabolism.[26] Ole D Wolthers reported that bilastine stands out among antihistamines for its non-sedating properties, making it an attractive option for patients who need relief from allergic symptoms without experiencing drowsiness or impairment in daily activities. This advantage enhances patient compliance and improves the overall quality of life.[11] Farre et al. reported that the significant advantage of bilastine was its favorable safety profile, particularly concerning its minimal potential for adverse effects on organs such as the heart and liver. This feature makes bilastine suitable for long-term use in patients with AR, including those with comorbidities.[27]
In a study conducted in the Vienna Challenge Chamber, it was found that the effect of bilastine started within an hour of receiving the drug, as indicated by the first significant reduction (P <0.05) in the total nasal symptom score after drug administration.[28] Church et al. reported that bilastine was quickly absorbed orally, with an oral bioavailability of 60%. The drug reaches maximum plasma concentrations within 1 to 1.5 hours and does not undergo significant hepatic metabolism. Approximately 95% of the drug was excreted unchanged, with 67% eliminated in feces and 33% in urine.[29]
The survey respondents also reported a preference for antihistamines in combination with montelukast for persistent AR. A comparative study by Mahatme et al. demonstrated that combination therapy of montelukast with antihistamines provides enhancing and complementary effects, contributing to effective symptom reduction.[30] Combining an antihistamine like bilastine with montelukast can be an effective treatment option for patients with AR. This combination therapy was particularly useful for patients who require both types of drugs to achieve better results.[31] Sinha et al. concluded that the combination of antihistamines (bilastine) and montelukast was effective and well-tolerated in Indian patients with AR. [32]
The survey results provide valuable insights regarding the trends and preferences in AR management, which may help enhance patient care and customize treatment strategies. One of the major strengths of the study was the use of a carefully designed and validated questionnaire to gather expert data. However, it was important to note that personal perspectives and preferences could have influenced the conclusion, and as such, the dependence on expert judgments increases the likelihood of bias. Therefore, it was necessary to examine the results while keeping these limitations in mind. Additionally, further research should be conducted to confirm and expand on the scope of the current survey findings.
Conclusion
The study results highlighted the preference for antihistamines, particularly bilastine, in managing AR due to its non-sedative properties. Bilastine has a favorable pharmacokinetic and efficacy profile, making it the preferred medication for treating AR. Additionally, clinicians preferred using a combination of antihistamines and montelukast to treat persistent AR in patients.
Source of funding
None.
Conflict of Interest
Nothing to declare.
Acknowledgement
We would like to thank all the clinicians who were participated in this study.
References
- M Egan, S Bunyavanich. Allergic rhinitis: the "Ghost Diagnosis" in patients with asthma. Asthma Res Pract 2015. [Google Scholar] [Crossref]
- S Akhouri, SA House. Allergic Rhinitis. 2023. [Google Scholar]
- SM Adsule, D Misra. Long term treatment with montelukast and levocetirizine combination in persistent allergic rhinitis: review of recent evidence. J Indian Med Assoc 2010. [Google Scholar]
- D Chandrika. Allergic rhinitis in India: an overview. Int J Otorhinolaryngol Head Neck Surg 2017. [Google Scholar]
- V Jaggi, A Dalal, BR Ramesh, S Tikkiwal, A Chaudhry, N Kothari. Coexistence of allergic rhinitis and asthma in Indian patients: The CARAS survey. Lung India 2019. [Google Scholar]
- RS Kumar, MK Jain, JS Kushwaha, S Patil, V Patil, S Ghatak. Efficacy and Safety of Fluticasone Furoate and Oxymetazoline Nasal Spray: A Novel First Fixed Dose Combination for the Management of Allergic Rhinitis with Nasal Congestion. J Asthma Allergy 2022. [Google Scholar] [Crossref]
- V Gupta, PS Matreja. Efficacy of montelukast and levocetirizine as treatment for allergic rhinitis. J Allergy Ther 2010. [Google Scholar] [Crossref]
- JM Sanjana, PA Mahesh, BS Jayaraj, KS Lokesh. Changing trends in the prevalence of asthma and allergic rhinitis in children in Mysore, South India. Eur Respir J 2014. [Google Scholar]
- DY Wang, AG Ghoshal, ARBA Muttalif, L Horng-Chyuan, S Thanaviratananich, S Bagga. Quality of Life and Economic Burden of Respiratory Disease in Asia-Pacific-Asia-Pacific Burden of Respiratory Diseases Study. Value Health Reg Issues 2016. [Google Scholar] [Crossref]
- H Kawauchi, K Yanai, D Y Wang, K Itahashi, K Okubo. Antihistamines for Allergic Rhinitis Treatment from the Viewpoint of Nonsedative Properties. Int J Mol Sci 2019. [Google Scholar] [Crossref]
- OD Wolthers. Bilastine: A new nonsedating oral H1 antihistamine for treatment of allergic rhinoconjunctivitis and urticaria. Biomed Res Int 2013. [Google Scholar] [Crossref]
- S Linton, L Hossenbaccus, A K Ellis. Evidence-based use of antihistamines for treatment of allergic conditions. Ann Allergy Asthma Immunol 2023. [Google Scholar]
- KL Craun, P Patel, MP Schury. . Fexofenadine. [Updated 2024 Feb 8] 2024. [Google Scholar]
- E Ridolo, M Montagni, L Bonzano, C Incorvaia, G W Canonica. Bilastine: new insight into antihistamine treatment. Clin Mol Allergy 2015. [Google Scholar] [Crossref]
- M Kiran, L Pawaskar, S Sheikh, P Waghambare. Efficacy and Safety for the combination of Montelukast and Levocetirizine in patients of allergic rhinitis: Post Marketing Surveillance study. Ann Int Med Dent Res 2021. [Google Scholar]
- A Baççıoğlu, A Yorgancioglu, C Cingi, Ç Çuhadaroglu. Role of leukotriene antagonists and antihistamines in treatment of allergic rhinitis and asthma comorbidity. J Med Updates 2013. [Google Scholar]
- M Ciebiada, M Górska-Ciebiada, L M Dubuske, P Górski. Montelukast with desloratadine or levocetirizine for the treatment of persistent allergic rhinitis. Ann Allergy Asthma Immunol 2006. [Google Scholar]
- J Bousquet, I Ansótegui, GW Canonica, T Zuberbier, CE Baena-Cagnani, C Bachert. Establishing the place in therapy of bilastine in the treatment of allergic rhinitis according to ARIA: evidence review. Curr Med Res Opin 2012. [Google Scholar]
- AS Randhawa, NM Noor, MKM Daud, B Abdullah. Efficacy and Safety of Bilastine in the Treatment of Allergic Rhinitis: A Systematic Review and Meta-analysis. Front Pharmacol 2022. [Google Scholar] [Crossref]
- S Bhagat, S Patil, S Panchal, H Barkate. Physicians perception in the management of allergic rhinitis: a Pan-India survey. Int J Otorhinolaryngol Head Neck Surg 2020. [Google Scholar]
- EO Meltzer, NA Rosario, HV Bever, L Lucio. Fexofenadine: review of safety, efficacy and unmet needs in children with allergic rhinitis. Allergy Asthma Clin Immunol 2021. [Google Scholar] [Crossref]
- AP Ten Eick, JL Blumer, MD Reed. Safety of antihistamines in children. Drug Saf 2001. [Google Scholar]
- MS Blaiss. Allergic rhinitis: Direct and indirect costs. Allergy Asthma Proc 2010. [Google Scholar]
- J Bousquet, N Demarteau, J Mullol, MEVD Akker-Van Marle, EV Ganse, C Bachert. Costs associated with persistent allergic rhinitis are reduced by levocetirizine. Allergy 2005. [Google Scholar]
- A Singh, H Kumar. Cost-analysis study of second generation antihistamines used in the treatment of allergic rhinitis in India. Int J Basic Clin Pharmacol 2016. [Google Scholar]
- I Jáuregui, J G Ramaekers, K Yanai, M Farré, E Redondo, R Valiente. Bilastine: a new antihistamine with an optimal benefit-to-risk ratio for safety during driving. Expert Opin Drug Saf 2016. [Google Scholar]
- M Farré, C Pérez-Mañá, E Papaseit, E Menoyo, M Pérez, S Martin. Bilastine vs. hydroxyzine: occupation of brain histamine H1-receptors evaluated by positron emission tomography in healthy volunteers. Br J Clin Pharmacol 2014. [Google Scholar]
- F Horak, P Zieglmayer, R Zieglmayer, P Lemell. The effects of bilastine compared with cetirizine, fexofenadine, and placebo on allergen-induced nasal and ocular symptoms in patients exposed to aeroallergen in the Vienna Challenge Chamber. Inflamm Res 2010. [Google Scholar]
- MK Church, M Tiongco-Recto, E Ridolo, Z Novák. Bilastine: A lifetime companion for the treatment of allergies. Curr Med Res Opin 2020. [Google Scholar]
- MS Mahatme, GN Dakhale, K Tadke, SK Hiware, SD Dudhgaonkar, S Wankhede. Comparison of efficacy, safety, and cost-effectiveness of montelukast-levocetirizine and montelukast-fexofenadine in patients of allergic rhinitis: A randomized, double-blind clinical trial. Indian J Pharmacol 2016. [Google Scholar]
- S Jain, S Verma, S Balamurugan, KRBK Reddy, DJ Christopher. Expert opinion on the role of bilastine and bilastine-montelukast combination in the management of allergic rhinitis: An Indian perspective. J Assoc Chest Physicians 2023. [Google Scholar]
- SD Sinha, S Perapogu, SS Chary, S Ramesh, J Bakshi, A Singh. Efficacy and safety of fixed-dose combination of Bilastine-Montelukast in adult patients with allergic rhinitis: a phase III, randomized, multi-center, double-blind, active controlled clinical study. J Asthma 2023. [Google Scholar]
