Introduction
Sarcomas are rare entities comprising 1% of all malignant tumors in adults. Being mesenchymal in nature they commonly develop in skin, fat, muscle, blood vessels, fibrous or nerve tissues. 1 Sarcoma of the chest wall is even rarer entity contributing to 10-15% of these tumor. 1 Pleomorphic liposarcoma is an aggressive adipocytic sarcoma of bone or soft tissues clinically presenting as swelling, pain, pathological fracture and occasional systemic features. These are characterized by high local recurrence and significant metastasis. Diagnosis is supported by chest radiograph and computed tomography scan. 1 Immunohistochemistry is quite important in differentiating these tumors from other tumors in view of confusing pathological picture at times. The management approach includes wide surgical resection of tumor with tumor-free margins followed by skeletal reconstruction and soft tissue coverage. 2 Like most cancers, the incidence of liposarcoma increases with advancing age, and subtotal resection can be considered a palliative surgical procedure. Herein, we present a case of pleomorphic liposarcoma of anterior chest wall which was diagnosed as a desmoid tumor during pre-surgical work-up. Immunohistochemistry revealed its true nature.
Case Report
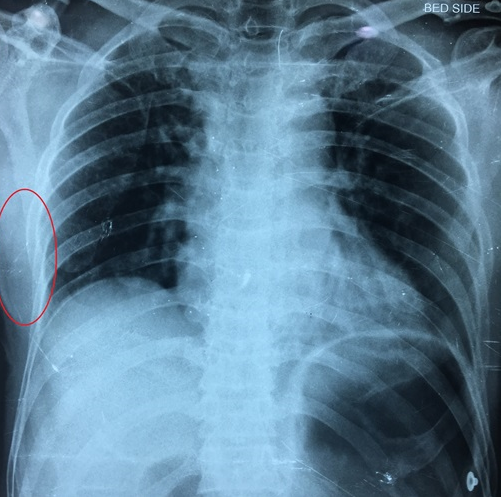
A 50-year-old non-smoker male farmer presented to the outpatient department with complaint of a swelling over right anterior chest wall for past 2 months. The swelling was gradually increasing in size, associated with dull aching pain. There was no history of breathlessness, cough, hemoptysis, fever, weight loss or trauma. On clinical examination, the patient had pulse rate of 82 beats per minute, blood pressure of 110/70 mm Hg, with a respiratory rate of 18/minute he was maintaining an oxygen saturation of 97% on room air. Chest examination revealed a swelling in right lower anterior chest wall measuring 3cmX2cm (Figure 1). Swelling was hard, non-tender, non-fluctuant in nature with normal overlying skin. Rest of respiratory system examination revealed no abnormal findings.
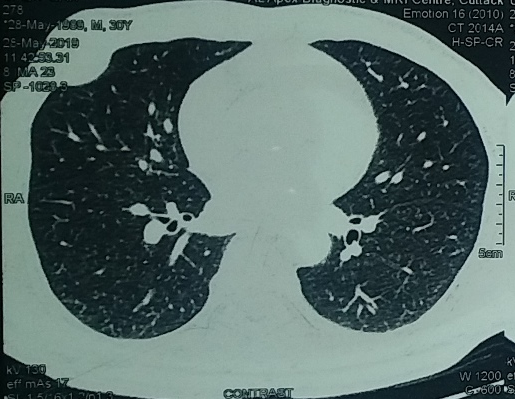
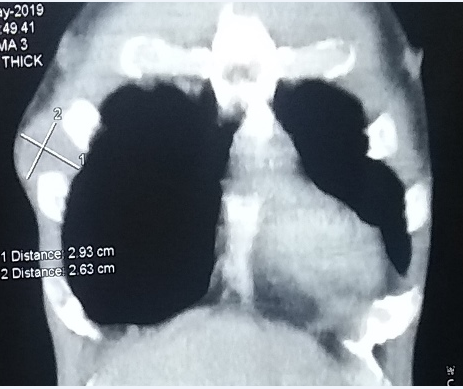
Chest radiograph showed a homogeneous shadow involving the soft tissue on the right without any parenchymal or skeletal structure involvement (Figure 2). The CT scan of chest showed a soft tissue density lesion in the anterior chest, there was no evident destruction/erosion in the adjacent ribs. Abnormal mediastinal nodes were not detected (Figure 3, Figure 4). USG abdomen ruled out presence of any synchronous mass, organomegaly or lymphadenopathy. FNAC done from chest wall mass showed benign spindle shaped cells with few round to oval cells giving an impression of benign spindle cell lesion. However tru-cut biopsy from the mass revealed spindle cells in fascicles with hyperchromatic pleomorphic nuclei suggestive of deep musculoaponeuritic fibromatosis (desmoid tumor). Wide local excision of chest wall tumor was done under general anesthesia and sent for histopathological examination (Figure 5).
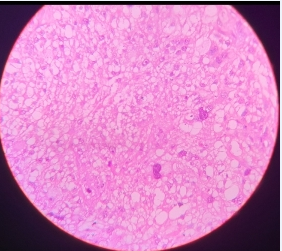
Histopathology revealed predominant spindle shaped cells with plump nuclei & conspicious prominent nucleoli. There was presence of atypical mitosis, bizarre cells, tumor giant cells and numerous mitotic figures (Figure 6) Necrosis and hyalinization were seen extensively. Tumor cells were positive for Vimentin and CD68 and negative for CD-34, S-100, SMA, Desmin, AE1/AE3 and D-240 all suggestive of pleomorphic liposarcoma.
Patient’s postoperative course was uneventful. Patient was referred to Oncology where he received radiation therapy. A written consent was taken from the patient for utilizing his clinical data and investigations.
Discussion
Liposarcoma is the second most common type of soft tissue sarcoma and accounts for approximately 15–20% of all reported sarcomas. 1 Pleomorphic liposarcoma represents the rarest of lipomatous malignancies, accounting for no more than 5% of all liposarcomas. 3 It slightly predominates in men, most frequently involving the lower extremity, particularly the thigh, followed by the upper extremity and the retroperitoneum. 4 Unusual sites include the mediastinum, paratesticular area, scalp (and other subcutaneous sites), abdominal cavity, pelvic cavity, orbit, and thorax. 5, 6 Nearly 70% of primary chest-wall soft-tissue sarcomas are low grade, and complete surgical excision is the preferred therapeutic choice. 7 Liposarcomas originate from primitive mesenchymal cells and are further classified into five categories: well-differentiated, myxoid, pleomorphic, round cell, and dedifferentiated. 8 A mutation in chromosome band 12q13 has been linked to the development of liposarcoma, which involves a chromosomal translocation of the FUS-CHOP fusion gene 9 Patients are usually asymptomatic, and symptoms are dependent on local invasion of organs. Some individuals present with pain as a result of compression of neurovascular structures, whereas if there is pleural, lung, or mediastinal invasion patients may present with shortness of breath. Here, the patient reported precordial chest pain for one month, easy fatigability. Pleural sarcomas are insidious and are not accessible on examination. 10 Metastasis to the pleura, mediastinal lymph nodes, lungs, kidneys, adrenal glands, and bone has been reported. 10 On CT scans, the appearance of liposarcomas varies from a predominantly fat‑containing lesion to a solid mass. They are heterogeneous depending on the amount of necrosis, calcification, vascularity, cystic changes, and soft‑tissue. Patients with primary soft‑tissue sarcomas of the chest wall after resection have survival rates similar to that of patients with sarcomas of the extremities. 10 The tumor subtype mostly determines the prognosis as dedifferentiated and pleomorphic subtypes are associated with recurrence and metastasis whereas patients with tumors which are well differentiated respond relatively better during follow‑ups. Our case was thus unique in being a pleomorphic subtype of liposarcoma, arising primarily in the anterior chest wall, but without noticeable involvement of mediastinal structures or distant metastasis in spite of being a higher‑grade. Furthermore, the importance of doing an immunohistochemistry despite getting a report with absence of atypia is highlighted here as the resection specimen showed a completely different picture on histopathology as well as immunohistochemistry in comparison to the initial trucut biopsy reports.