Introduction
Obstructive sleep apnea (OSA) may affect nearly 20 percent of obese pregnant women.1 Hypertensive disorders of pregnancy, Gestational diabetes mellitus and cardiomyopathy are the major comorbidities associated with OSA in pregnancy. It has been well documented that OSA in pregnancy have 2-fold increased risk of developing preeclampsia and 1.5-3.5-fold increased risk of the developing of gestational diabetes mellitus. 2
Obstructive sleep apnea is a major public health concern which increases the cardiovascular and cerebrovascular comorbidities. OSA screening is mandatory for specific population which includes obese people, patients with Resistant /poorly controlled diabetes mellitus/hypertension and Chronic kidney diseases. Even though lot of pathophysiological factors increases the risk of OSA in pregnancy, available literature in these group of population is sparse.
Adverse fetomaternal outcomes were well documented in patients with OSA in pregnancy. Hence it is mandatory to screen these patients which is a challenging task. Polysomnography is the gold standard investigation for the diagnosis of OSA but limited by its cost, waiting period in health care setting with significant patient load and time consumption. Unattended level 3 home based sleep studies is emerging as reliable cost-effective method for diagnosing OSA in high clinical suspicions.
The snoring, tiredness, observed apnea, high Blood pressure, Body mass index(BMI), age, neck circumference, and male gender (STOP-Bang) questionnaire was specifically developed to meet the need for a reliable, concise, and easy-to-use screening tool for OSA. It consists of eight dichotomous (yes/no) items related to the clinical features of sleep apnea. The total score ranges from 0 to 8.
So the purpose of our study was to assess the prevalence of risks of OSA in obese pregnant ladies by using established STOP BANG Questionnaire.
Materials and Methods
Sample size
Sample size was calculated based on the prevalence and study subjects from the previous study using free cal software.3
Exclusion criteria
Pregnant women with Thyroid dysfunction.
Pregnant women with craniofacial abnormalities.
Pregnant women with Upper airway pathology.
Patients who are unwilling to participate in our study.
21 Obese pregnant women were recruited in our present study after fulfilling inclusion criteria and exclusion criteria. The study was conducted after approval from institutional ethical committee. Written informed consent was taken from all of them. After collecting demographic details of each patient, Patient was examined. Neck circumference in centimeters /inches and BMI(weight/height in meter square) were recorded .Relevant investigation were sent to apply execution criteria. Risk of OSA was assessed using STOP BANG questionnare. All the data was entered and analysed with epi info software version 3.4.3.
Results
21 obese pregnant women were included in our study. The mean age of our study population was 29.5years. All of them were from rural areas in the region of Puducherry.70 % of the study population belong to poor socioeconomic status as per Kuppusamy scale.
Out of 21 obese pregnant women, 66%(n=14) were multigravida and 34% were primigravida.10 % of them had history of previous abortions.
5 (23.8%) of them had Pregnancy induced hypertension 7(33 3% had gestational diabetes.
Regarding symptoms pertaining to OSA, most of them had snoring (n=18, 85.7%) followed by day time sleepiness (n=15,71.4%), Day time tiredness (n=14, 66.6%) Early morning headache (n=6, 28.5%) and chocking episodes (n=4,19%), and nocturnal enuresis in 2 patients.
66.6%(n=14)of the study population had BMI in the range 30-35 whereas 28.6%(n=6) had BMI between 35 to 40. one patient had morbid obesity with BMI more than 40.
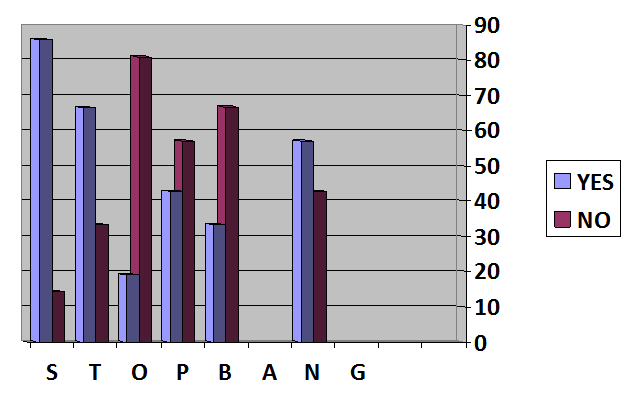
With regard to stop bang questionnare, Most of the study subjects (85.7%) had history of snoring both reported by them and their bed partners. History of tiredness was reported by 14 patients (66.6%). chocking or history of gasping was reported by only 4 patients (19%). 4 of them had systemic hypertension and 5 patients had pregnancy induced hypertension.
13(61.9%) patients had BMI greater than 35. Question pertaining to age and sex in questionnare is not applicable for our study population.
Table 1
Distribution of Study subjects based on Body mass index
| BMI | n(%) |
| 30-35 | 14(66.6) |
| 35-40 | 6(28.6) |
| 40 | 1(4.8) |
Table 2
Scoring of stop bang questionnare
Discussion
This cross sectional study on assessment of obstructive sleep apnea risk among the obese pregnant women was done in tertiary care centre in the rural population of Puducherry.
Results of our study showed that 42.9% of the obese pregnant women had high risk, 42.9% had intermediate risk and 14.3% for OSA as per the STOP BANG scoring.Thus most of our study subjects were having higher risk of OSA which needed further evaluation with polysomnography.
Chung et al4 showed STOP-BANG with specific combinations of individual components in the questionarre improved the specificity. Patients with a STOP score of ≥ 2, male gender and a BMI greater than 35 kg/m2 were more predictive of OSA than age greater or equal to 50 and neck circumference > 40 cm. So, a screening tool is much needed which should be specific for the women in pregnancy to diagnose OSA.
Haulek Mergan et al5 in their study with 217 obese patients, scoring cut off 3-4 provides a better balance of sensitivity and specificity for all OSA.
9 patients had hypertension in our study population among the obese pregnant women. Previous studies showed high incidence of Ischemic heart disease, systemic hypertension, stroke, Acid peptic disease, heart failure with OSA.6, 7
Jennifer E. Dominguez et al 8 in their study noted that higher total STOP-BANG score was clearly linked with high likelihood of pre-pregnancy and pregnancy-induced hypertension with diabetes mellitus which is similar to our study.42.8% of our study subjects were hypertensive with higher STOP BANG scores.
STOP‐BANG was the most commonly used screening tool among the departments that screened for OSA.9
Similar studies with the use of STOPBANG in the first and third trimesters of pregnancy concluded that even though it had a good negative predictive value, the score was not useful for detecting OSA.9, 10, 11, 12, 13 Tantrakul et al14 studied the usage of STOPBANG questionnaire in 72 women across trimesters and found it to have the best predictive value during the second trimester.
In our study, 12 patients (57.1%) had neck circumference more than 16 inches. In a study by Fiona Pearson et al 15 41% of study patients had neck circumference greater than 40 cm.
Most of the obese pregnant women (87.5%) in our study reported snoring. Other authors have described snoring rates of 17-34% in pregnancy but not in obese pregnant women 16, 17. Snoring was prevalent in our study this may be due to the fact that other similar studies concentrated on snoring conducted detailed interviews with precise criteria for snoring, whereas our study used simple self-reporting with the help STOP BANG questionnaire. Smith et al 18 suggested that habitual snoring (snoring at 14 least 3 nights per week) could be used as a triage tool for OSA in pregnancy, especially among those with a BMI≥40.
A large proportion of study population reported day time sleepiness (71.4%) and tiredness (66.6%) which is similar to a study by Fiona Pearson et al. 15 Patients also had history of choking episodes which is predominantly seen in patients with BMI greater than 35. Few patients reported early morning headache and nocturnal enuresis.
Thus patients with higher BMI, neck circumference more than 16 inches with higher reporting of snoring and tiredness invariably had higher STOP BANG scores which shows these group of patients have high risk of developing obstructive sleep apnea in pregnancy like in general population, However these patients should be referred for polysomnography to confirm the diagnosis of Obstructive sleep apnea.
Conclusion
This study showed higher prevalence of risks for OSA in obese pregnant women as per STOP BANG questionnare which can be utilised for screening OSA in these group of patients. However it requires meticulous history taking and scoring with the questionnare which in turn requires measurements that are not normally done in an antenatal outpatient department. Scoring of STOP BANG questionnaire is much simpler and less time consuming when compared to other questionnaires to assess the risk of OSA. Thus Obese pregnant women reporting loud and frequent snoring with day time tiredness and comorbidities should be referred for investigation of obstructive sleep apnea. However, Multicentric studies with large sample size should be initiated using Level 1 or Level 2 Sleep study in obese women with the aim of developing a pregnancy-specific screening tool for OSA.