- Visibility 450 Views
- Downloads 94 Downloads
- Permissions
- DOI 10.18231/j.ijirm.2024.028
-
CrossMark
- Citation
Practice of cough etiquette and quality of life among MDR-TB patients at a tertiary care hospital
Abstract
Background: Tuberculosis is a highly contagious disease. When a patient with pulmonary TB coughs/sneezes without appropriate cough etiquette, it may spread to others. Also cough due to TB has significantly impaired quality of life of patient.
Aims and Objectives: To find the cough hygiene practices and assess quality of life among multi drug resistant tuberculosis patients.
Materials and Methods: It was a hospital based cross-sectional study conducted at DR-TB centre of Basaveshwara medical college and hospital over a period of six months. All the active MDR-TB cases either attending or admitted at the DR-TB centre were personally interviewed by giving preformed questionnaire to assess the knowledge and practice of respiratory hygiene and Leicester cough questionnaire and Cough specific quality of life questionnaire were given to assess the quality of life.
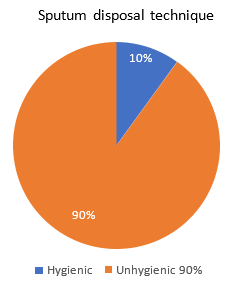
Results: Total of 50 patients were included in our study out of which 28 were males and 22 were females. Majority (64%) were unaware of mode of transmission of TB. 90% were unaware of hygienic sputum disposal. Knowledge and practice of cough etiquette was poor. Our study also showed that total LCQ scores were lower in females as compared to males (10.1±2.8 versus 12.3±2.2). Total CQLQ scores were higher in females as compared to males (78.3±10 versus 69.6±4.9). Both indicating worse QOL in female patients.
Conclusion: Majority were unaware of proper knowledge and practice of cough hygiene. Most of the females reported worse QOL. There should be proper interaction between DOTS providers and patient’s, they should educate patients about cough etiquette and its importance. NTEP should also focus on improving QOL of patients.
Introduction
Tuberculosis is a leading cause of mortality and morbidity from infectious disease globally and drug-resistant forms of tuberculosis are a threat to global health security.[1] Covid-19 is having a major impact on MDR-TB in India through their effect mainly on TB diagnosis and treatment. Globally, a 3-month lockdown and a protracted 10-month restoration could lead to an additional 6.3 million cases of TB between 2020 and 2025, and an additional 1.4 million TB deaths during this time.[2] India accounts for about quarter of global TB burden. This amounts to about 2.6 million cases out of 10 million cases worldwide. It also led to the death 9,500 HIV positive people and 436,000 HIV negative people in our country.[3] India has the highest burden of MDR-TB in the world, it had an estimated 130,000 drug resistant TB cases in 2018.
Globally in 2019, an estimated 10.0 million people fell ill with TB. There were 1.2 million TB deaths among HIV-negative people and an additional 208 000 deaths among HIV- positive people. In 2019, an estimated 3.3% of new TB cases and 18% of previously treated cases had MDR/RR-TB. In absolute numbers, there were an estimated 465 000 incident cases of Rifampicin-resistant TB; 78% had multidrug resistant TB. [4]
Tuberculosis diagnosis and treatment currently revolves around clinical features and microbiology. The disease however adversely affects patients’ psychological, economic, and social well-being as well, and therefore our focus also additionally needs to shift towards quality of life (QOL). The disease influences all QOL domains and substantially adds to patient morbidity, and these complex and multidimensional interactions pose challenges in accurately quantifying impairment in QOL. [5]
Cough etiquette refers to series of action to take while coughing or sneezing which are designed to reduce the spread of respiratory illness to other. Cough hygiene refers to measures like 1) cover the mouth/ nose when coughing or sneezing 2) Use in the nearest waste receptacle to dispose of the tissue after use 3) Perform hand hygiene after having contact with respiratory secretions and contaminated objects/materials. Cough hygiene is one among the five steps for “Patient Management to Prevent Transmission of TB in Health Care Settings” as recommended by WHO. [6]
With this background, the present study was undertaken to evaluate the quality of life and assess the cough hygiene practices among MDR-TB patients at a tertiary care hospital in Central Karnataka.
Aims and Objectives
To assess the cough hygiene practice among MDR-TB patients.
To study the awareness, importance of cough hygiene and sputum disposal technique among MDR-TB patients
To assess the quality of life among MDR-TB patients. All of the above objectives were achieved.
Materials and Methods
It was a hospital based cross-sectional study at the drug-resistant tuberculosis management centre (DR-TB centre) of Basaveshwara medical college and hospital, Chitradurga for a period of Six months (20th March 2022 to 20th September 2022). Approval from institutional research and ethics committee was obtained and patients were recruited after informed consent.
Inclusion criteria
It was a complete enumeration of all the active MDR-TB cases attending DR-TB centre of Basaveshwara medical college and hospital, Chitradurga. All the MDR-TB cases either admitted or attending and those who are willing to participate in the study during the study period were included after obtaining the informed consent. These patients were personally interviewed based on the questionnaire prepared.
Exclusion criteria
MDR-TB patients who did not give consent, health care workers, medical professionals and patients with co-morbid conditions such as malignancy, HIV, psychiatric diseases were excluded from the study.
Questionnaires
All the relevant clinico-demographic data such as age, sex, current residence, education and occupation was obtained.
Questionnaires to assess cough practice: Questionnaires were structured with help of senior pulmonologist in the respiratory medicine department of hospital and it mainly concentrated on the knowledge of spread of TB, covering of mouth and nose while coughing and sneezing, use of alternatives if mask or napkin is not available, sputum disposal practice, washing of hands after coughing, awareness of hazards of indiscriminate sputum disposal.
Questionnaires to assess quality of life: Leicester cough questionnaire (LCQ) and cough specific quality of life questionnaire (CQLQ) were used, both the questionnaires are well validated in general population.
Leicester cough questionnaire (LCQ)
It consists of 19 questions that are divided into three domains as described in [Table 1]:
|
Physical domain |
Q, Q2, Q3, Q9, Q10, Q11, Q14, Q15 |
|
Psychological domain |
Q4, Q5, Q6, Q12, Q13, Q16, Q17 |
|
Social domain |
Q7, Q8, Q18, Q19 |
Domain scores: total scores from items in domain/number of items in domain (range 1-7) Total scores: addition of domain scores [range 3-21]
It is a 7-point Likert scale. It assesses the impact of cough over preceding 2 weeks. The total score ranges from 3-21; a higher score corresponds to a better health status [7].
Cough specific quality of life (CQLQ)
It has 28 questions divided into six subscales ([Table 2])
|
Physical complaints |
Q4, Q8, Q10, Q13, Q14, Q15, Q17, Q22, Q23 |
|
Psychosocial issues |
Q1, Q18, Q24, Q25, Q27 |
|
Functional abilities |
Q2, Q3, Q19, Q20, Q21 |
|
Emotional well being |
Q7, Q9, Q12, Q16 |
|
Extreme physical complaints |
Q5, Q6, Q11, Q12 |
|
Personal safety fears |
Q9, Q26, Q28 |
Only two items 9 and 12 overlapped subscales. Item 9 appears in the emotional wellbeing and personal safety fears subscales, item 12 appears in emotional wellbeing and extreme physical complaints subscales.
CQLQ is a 4-point Likert scale (1-strongly disagree, 2-disagree, 3- agree, 4-strongly agree)
Scoring: The total score is the sum of all individual items. Subscales cores are the sum of items identified for each scale.
The lowest possible achievable total score indicating no adverse effects of cough on quality of life is 28 and the highest possible total score is 112 [8]
Data analysis
Data was entered and compiled by using Microsoft Excel. Data was analysed using statistical package for social science (SPSS).
Results
|
Study variables |
Frequency (n=50) |
Percentage (%) |
|
Sex |
|
|
|
Male |
28 |
56 |
|
Female |
22 |
44 |
|
Education |
|
|
|
Primary (class 1 to 5) |
20 |
40 |
|
Upper primary (class 6to8) |
12 |
24 |
|
Secondary (class 9 to 10) |
10 |
20 |
|
Upper secondary (class11to 12) |
4 |
8 |
|
Higher education |
4 |
8 |
|
Total members in the household of patients |
|
|
|
Staying alone |
1 |
2 |
|
Less than 5 |
36 |
72 |
|
More than 5 |
13 |
26 |
|
Total number of rooms in the patient’s house |
|
|
|
1 |
34 |
68 |
|
2 |
15 |
30 |
|
3 |
1 |
2 |
|
Total |
50 |
100 |
A total of 50 multi drug resistant tuberculosis patients who fulfilled the study criteria, participated in the study.
[Table 3] describes the socio-demographic profile of the MDRTB patients. 56% were males and 44% were females.
A majority of 40% of patients had studied up-to primary school. A 24% had studied up-to upper-primary, 20% had secondary education, whereas 8% had studied upper secondary and higher education.
A 72% of patients belonged to families with less than 5members per household And 26% lived in joint families with more than 5 members per household. One patient was staying alone.
Only 1 room was present in majority of 68% of the houses of patients, 30% patients lived in houses with 2 rooms.
|
Study variables |
Frequency (n=50) |
Percentage (%) |
|
Awareness of mode of transmission of MDR-TB |
|
|
|
Present |
18 |
36 |
|
Absent |
32 |
64 |
|
Awareness of hazards of indiscriminate sputum disposal |
|
|
|
Present |
15 |
30 |
|
Absent |
35 |
70 |
|
Awareness about alternatives if face masks or napkin are not available |
|
|
|
Present |
20 |
40 |
|
Absent |
30 |
60 |
|
Total |
50 |
100 |
[Table 4] depicts the knowledge of respiratory hygiene among MDR-TB patients
In the study it was found that majority 32(64%) were unaware of mode of transmission of MDR-TB ([Table 4]), only 18 (36%) were aware that it spreads through air when infected person coughs or sneezes without following appropriate cough etiquette and MDR-TB is a drug resistant form of pulmonary tuberculosis.
The study also showed that majority 35 (70%) were not aware of hazards of indiscriminate sputum disposal.([Table 4])
The study also showed that majority of MDR-TB patients 30 (60%) were not aware of alternatives if facemask/ hand kerchief is not available that is to use cough or sneeze over elbow or upper sleeves.([Table 4])
|
Study variables |
Frequency (n=50) |
Percentage (%) |
|
|
|
|
|
Covering of mouth and nose while coughing or sneezing |
|
|
|
Practised regularly |
45 |
90 |
|
Irregular |
5 |
10 |
|
The procedure to cover mouth while coughing or sneezing |
|
|
|
Using handkerchief |
21 |
42 |
|
Using Face masks |
22 |
44 |
|
Using tissue paper or handkerchief |
5 |
10 |
|
Others |
2 |
4 |
|
Adherence to Treatment regimen |
|
|
|
Present |
47 |
94 |
|
Absent |
3 |
6 |
|
Usage of facemasks or handkerchiefs in public places |
|
|
|
Practiced regularly |
47 |
94 |
|
Irregular |
3 |
6 |
|
Use of face-masks by the members of house-hold while interacting/ staying same room |
|
|
|
Present |
16 |
32 |
|
Absent |
34 |
68 |
|
Practice of washing hands after coughing or sneezing |
|
|
|
Present |
44 |
88 |
|
Absent |
6 |
12 |
|
Method of disposal of used face masks? |
|
|
|
Replacing with new one |
14 |
28 |
|
Washing and reusing them again |
36 |
72 |
|
Methods of disposal of sputum |
|
|
|
Hygienic include only |
5 |
10 |
|
Unhygienic |
45 |
90% |
|
Total |
50 |
100 |
[Table 5] shows the practice of respiratory hygiene and adherence to MDR-TB treatment regimen. In the study it was found that majority 45(90%) MDR-TB patients practiced covering ofmouth and nose while coughing or sneezing and most them used handkerchief and facemask that is 42% and 44% respectively and 94% patients regularly used facemask or handkerchief in public places.
Adherence to the MDRTB drug regimen was seen among 94% patients, whereas 6% patients were non-adherent to the treatment regimen.
Practice of washing hands after coughing or sneezing was reportedly followed by 88% of patients.
In the study it was also found that majority 90% of MDR-TB patients practiced unhygienic sputum disposal technique, that is they spitted indiscriminately in open space and only 10% of patients used open/closed containers and practiced hygienic sputum disposal ([Figure 1])
|
Knowledge and practice of respiratory hygiene among the patients |
Education |
P value |
||
|
Up-to primary school |
Up-to Secondary / PUC/ Degree |
Total n (%) |
|
|
|
|
n(%) |
n(%) |
|
|
|
Knowledge about modes of transmission of PTB |
|
|
|
|
|
Absent |
25 (78.1%) |
7 (21.9%) |
32 (100.0%) |
0.006 |
|
Present |
7 (38.9%) |
11 (61.1%) |
18 (100.0%) |
|
|
Adherence to medication advice |
|
|
|
|
|
Absent |
2(66.7%) |
1(33.3%) |
3(100%) |
0.921 |
|
Present |
30(63.8%) |
17(36.2%) |
47(100.0%) |
|
|
Coveringmouth/ nose While coughing or sneezing |
|
|
|
|
|
Not practiced |
4(80.0%) |
1(20.0%) |
5(100.0%) |
0.432 |
|
Practiced |
28(62.2%) |
17(37.8%) |
45(100.0%) |
|
|
Usage of face masks in public places |
|
|
|
|
|
Not practiced |
3(100.0%) |
0(0.0%) |
3(100.0%) |
0.180 |
|
Practiced |
29(61.7%) |
18(38.3%) |
47(100.0%) |
|
|
Washing hands after coughing sneezing |
|
|
|
|
|
Absent |
5(83.3%) |
1(16.7%) |
6(100.0%) |
0.293 |
|
Present |
27(61.4%) |
17(38.6%) |
44(100.0%) |
|
|
Disposal of sputum |
|
|
|
|
|
In close containers |
1(20.0%) |
4(80.0%) |
5(100.0%) |
0.024 |
|
In open containers |
8(100.0%) |
0(0.0%) |
8(100.0%) |
|
|
Other |
1(100.0%) |
0(0.0%) |
1(100.0%) |
|
|
Spits in open |
22(61.1%) |
14(38.9%) |
36(100.0%) |
|
|
Awareness of hazards of indiscriminate sputum disposal? |
|
|
|
|
|
Awareness absent |
26(74.3%) |
9(25.7%) |
35(100.0%) |
0.021 |
|
Awareness present |
6(40.0%) |
9(60.0%) |
15(100.0%) |
|
[Table 6] depicts the association of knowledge and practice of respiratory hygiene with educationalstatus among the patients. In study it was found that majority of 61% of MDR TB patients who had education up-to secondary/pre-university/ degree levels had the knowledge about modes of transmission of MDR-TB when compared to the patients with primary level education (38.9%) and this association was found to be statistically significant (p value-0.006).
Accordingly, awareness of hazards of indiscriminate sputum disposal was significantly higher among patients with secondary or higher level of education (60%) compared to those with primary school education (40%) and this association was found to be statistically significant (p value-0.021)
Indiscriminate spitting in open places was practiced by 38.9% of patients with secondary/PU/degree level education compared to those with primary education (61.1%) and this association was found to be statistically significant (p value-0.024).
Adherence to medication advice was significantly higher among patients with primary schooling compared to those with higher education. But this association was not statistically significant (p value-0.921).
Adherence to medication advice (63.8%), practice of covering mouth and nose while coughing and sneezing (62.2%) and usage of face masks in public place on regular basis (61.7%) was higher among patients with primary schooling when compared to patients with secondary and higher education.
Assessment of quality of life among MDR-TB patients
|
Domains |
Mean |
SD |
|
Physical do main score |
3.6 |
1.0 |
|
Psychological do main score |
3.8 |
1.1 |
|
Social do main score |
4.0 |
0.9 |
|
Total score |
11.3 |
2.7 |
[Table 7] describes the average scores of patients as per LCQ questionnaire. The physical , psychological and social domain scores of the MDR TB patients was found to be 3.6 ±1.0, 3.8 ±1.1, 4.0 ±0.9 respectively.
The overall QOL score average was found to be 11.3±2.7.In our study it was also found that 28% of patients had to leave the job and 26% reported compromised work efficiency due to effected QOL.
|
Domains |
Mean |
SD |
|
Physical complaints score |
25.1 |
3.4 |
|
Psychosocial issues score |
12.2 |
1.8 |
|
Functional abilities score |
13.7 |
2.3 |
|
Emotional well-being score |
6.7 |
1.5 |
|
Extreme physical complaints score |
9.3 |
2.3 |
|
Personal safety fears score |
6.3 |
1.3 |
|
Total score |
73.4 |
8.7 |
The quality of life of the patients was also assessed by CQLQ questionnaire. The table 8 and Figure No. 6 describes the scores of individual subscales and total scores of the same. The average domain scores of patients were as follows:
Physical Complaints score was 25.1±3.4, Psychosocial issues score was 12.2±1.8, Functional abilities score was 13.7±2.3, Emotional wellbeing score 6.7±1.5, extreme physical complaints score was 9.3± 2.3 and personal safety fears score was 6.3±1.3.
The overall average of QOL as per CQLQ was found to be 73.4± 8.7
|
LCQ Domains |
Male |
Female |
p value* |
||
|
Mean |
SD |
Mean |
SD |
||
|
Physical domain score |
3.9 |
0.8 |
3.3 |
1.1 |
0.029 |
|
Psychological domain score |
4.2 |
0.8 |
3.3 |
1.2 |
0.004 |
|
Social domain score |
4.3 |
0.9 |
3.6 |
0.8 |
0.005 |
|
Total score |
12.3 |
2.2 |
10.1 |
2.8 |
0.004 |
[Table 9] shows the gender related difference on quality of life (QOL) by Leicester cough questionnaire (LCQ). Higher the LCQ score indicates better QOL. Females had the total score of 10.1±2.8 versus 12.3±2.2 in males (p value-0.004). Physical domain scores in female were 3.3±1.1 versus 3.9±0.8 in males (pvalue-0.029). Psychological domain scores in female were 3.3±1.2 versus 4.2±0.8 in males (p value-0.004). Social domain scores in female were 3.6±0.8 versus 4.3±0.9 in males (p value-0.005).
Score of all the three domains and total score was low in females as compared to males indicating worst QOL in females. All the three domains and total score showed statistical significance with p value less than 0.05 indicating males have better QOL as compared to females.
|
CQLQ Domains |
Male |
Female |
p value |
||
|
Mean |
SD |
Mean |
SD |
||
|
Physical Complaints score |
24.3 |
2.6 |
26.1 |
4.1 |
0.066 |
|
Psychosocial issues score |
11.6 |
1.1 |
13.0 |
2.3 |
0.008 |
|
Functional abilities score |
13.4 |
2.0 |
14.2 |
2.7 |
0.189 |
|
Emotional wellbeing score |
6.3 |
1.5 |
7.3 |
1.4 |
0.025 |
|
Extreme physical complaints score |
8.1 |
1.7 |
10.8 |
2.0 |
0.000 |
|
Personal safety fears score |
5.9 |
1.0 |
6.9 |
1.4 |
0.004 |
|
Total score |
69.6 |
4.9 |
78.3 |
10.0 |
0.000 |
[Table 10] shows the gender related difference on quality of life (QOL) by cough specific quality of life questionnaire (CQLQ). Higher the score indicates worse QOL. Females had an average total score of 78.3±10 versus 69.6±4.9 in males. Physical complaints score was 26.1±4.1 in females versus 24.3±2.6 in males. Psychosocial issue score was 13±2.3 in females versus 11.6±1.1 in males. Functional abilities score was 14.2±2.7 in females versus 13.4±2 in males. Emotional well-being score was 7.3±1.4 in females versus 6.3±1.5 in males. Extreme physical complaints score was 10.8±2 in females versus 8.1±1.7 in males.
Personal safety fear score was 6.9±1.4 in females versus 5.9±1 in males.
CQLQ questionnaires also highlighted about urinary incontinence. In our study it was found 9 out of 22 females had urinary incontinence, only 2 out of 28 males had urinary incontinence.
All the subscale scores and total score was comparatively higher in females as compared to males indicating worse QOL in females.
Psychosocial issues, emotional well-being, personal safety fears scores showed statistical significance (p<0.05) indicating worse QOL in females.
Extreme physical complaints and total score showed high statistical significance (p<0.001) indicating better QOL in males.
Other two subscales that are physical complaints and functional abilities score though showed worse QOL in females but did not statistical significance(p>0.05).
Discussion
The study was undertaken to assess the cough hygiene practices and QOL among MDR-TB patients.
Knowledge and practice of cough hygiene
In our study it was found that knowledge of mode of transmission of TB was poor. Only 36% were aware of mode of transmission. This result was similar to those of Cheriamane D, et al., which was conducted on the pulmonary tuberculosis patients. But this was in contrast to the study Sitapaudel where 64.5% were aware of communicability of the disease. [9]
90% respondents in our study showed unhygienic sputum disposal. This finding corroborates well with the findings of Venkatesh U et al., who reported unhygienic sputum disposal by 2/3rd patients at home and more than 90% at public places. [10] In study conducted by CheriamaneD et al., and Bhattacharyya et al., also reported unhygienic sputum disposal by majority of pulmonary tuberculosis patients, [11] In the study conducted by Bhatt G, et al indiscriminate spitting ofsputum was only 8.6%. [12] In the study conducted by Akshaya et al reported that 53.8% of the patients in there study were aware of appropriate method of sputum disposal. [13] The reason could be lack of awareness about the health hazards related to healthcare waste, inadequate training in proper waste management, absence of waste management and disposal systems, insufficient financial and human resources and the low priority. Many countries either do not have appropriate regulations, or do not monitor and enforce them. [14]
Patients should be provided individual containers with lid, containing 5% phenol, for collection of sputum and instructed on spitting the sputum directly in the container or in a tissue paper which is then thrown in the container. The container should be emptied daily and the sputum disposed off as per the infection control guideline. [15]
Biomedical waste refers to any waste produced by healthcare facilities that can negatively impact human health or the environment if not properly disposed of. This type of waste is deemed infectious and requires appropriate management which also includes proper disposal of sputum and masks.
Color-coded bags are used in TB labs to separate waste. The yellow bag is used for Truenat chips (MTB/RIF), used masks, and gowns. The red bag is used for specimen collection tubes, sputum cups, CBNAAT cartridges, infected plastic, contaminated tips, Pasteur pipettes, Truenat cartridges, PCR tubes, used gloves, MGIT tubes, and disposable LJ tubes. The blue bag is used for glass slides in the Truenat machine and used microscopy slides, making sure they are undamaged. Laboratories should keep abreast of changes to the regulations governing the treatment of biomedical waste.
Sputum disposal: Spittoons in the inpatient facility must be sanitized with 5% phenol for an hour before being emptied into the regular drain (ideally, an effluent treatment plant is present; if not, make sure the tap water is running). Spittoons can be reused after autoclaving and given to the patient once the 5% phenol disinfectant has been added. At the patient's residence, the contents must be drained and the spittoon boiled, which can be reused after adding the disinfectant (5% phenol). [15]
Seemingly in our study majorityof the MDR-TB patients (90%) covered their mouth while coughing. This is better than the findings of Bhatt G et al. [12]
Majority of the respondents in our study practiced regular hand washing after coughing. This finding is better than the findings of Venkatesh U, et al. [10]
Most of the respondents in our study were unaware of use of alternatives if facemask or handkerchief that is to cough on elbow or upper sleeves. Most of the respondents were unaware of safe sputum disposal.
Overall, the knowledge and practice of respiratory hygiene was poor in our study.
Assessment of quality of life
Cough is a prominent symptom of pulmonary TB. [16] It has a major impact on QOL of patients. In the study conducted by R Sharma et al by using WHO QoL method inferred that QOL of MDR-TB patients was lower than pulmonary TB. [16]
In our study we used LCQ and CQLQ questionnaire to assess the QOL in MDR-TB patients. Many of the items included are common to both questionnaires, confirming consistent themes in quality-of-life impairments, despite development in three different countries. [17]
LCQ was found to be relevant, comprehensive and useful in TB.[18] In our study it was found that 28% of patients had to leave the job and 26% reported compromised work efficiency due to effected QOL. It was similar to the findings of other studies R Sharma et al and Khan A et al. [16], [19]
Our study reported lower total LCQ scores and lower LCQ scores for all the three domains in females indicating worse QOL in females as compared to males and this was found to be statistically significant. The study conducted by Polley et al., also showed females are affected more due to cough as compared to males [20]. In contrast gender differences in QOL was not found by Kelsall et al. [21]
We also used CQLQ questionnaires to assess QOL. In our study it was found that total CQLQ scores and all six subscales’ scores were high in females indicating worse QOL in females as compared to males. CQLQ questionnaires also highlighted about urinary incontinence. In our study it was found 9 out of 22 females had urinary incontinence, only 2 out of 28 males had urinary incontinence. The study conducted by French et al., and Field et al., also showed that cough effected quality of life in females more as compared to males. [22], [23]
Overall, our study showed that cough had serious impact on females as compared to males both by LCQ and CQLQ. Hormonal influences may contribute to increased cough sensitivity in women, with factors such as laryngeal hypersensitivity and mast cell activity being implicated. [24] Psychological aspects, including anxiety and social embarrassment related to coughing, are more pronounced in females, affecting their daily lives and social interactions. [25] Hence, addressing stigma in the workplace through psychoeducation and support can significantly improve mental health outcomes and treatment adherence. [26] Involving family and community members in support initiatives can foster a more supportive environment for female patients undergoing treatment. [27]
Cough hygiene should be promoted through signage, equipment and practice ensured through patients and staff training, ongoing reinforcement by staff.
Patient education should be conducted on cough hygiene, etiquette, sputum disposal, proper use of surgical masks, restricted visitor entry at each admission and reinforced frequently by staff.
To maintain Cough hygiene, display signboards in the ward demonstrating cough hygiene. All patients admitted in the ward should be issued with surgical masks. Adequate measures should be taken for safe collection and disposal of sputum. [15]
Conclusion
Majority of the MDR-TB patients had poor knowledge about mode of transmission
Most of them were unaware about etiology, prevention, hygienic sputum disposal and proper cough etiquette.
DOTS providers are close to patients as compared to doctors as a result first all the agents should be educated about etiology, hygienic sputum disposal and proper cough etiquette and there should be proper interaction between DOTS agents and patients.
Quality of life was worse in female MDR-TB patients. Hence NTEP along with case detection and treatment should also focus on improving quality of life of patients.
Abbreviations
MDR-TB - Multidrug resistant tuberculosis; QOL - Quality of life: LCQ - Leicester cough questionnaire; CQLQ - Cough specific quality of life question; NTEP - National Tuberculosis Elimination Program.
Source of Funding
None.
Conflict of Interest
None.
References
- Floyd K, Glaziou P, Zumla A, Raviglione M. The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. Lancet Respir Med. 2018;6(4):299-314. [Google Scholar]
- . The potential impact of the covid-19 response on tuberculosis in high-burden countries: A modelling analysis. . . [Google Scholar]
- . TB Statistics India-2019, incidence, prevalence-TB Facts. . . [Google Scholar]
- Aggarwal A. Quality of Life with Tuberculosis. J Clin Tuberc Other Mycobact Dis. 2019;17. [Google Scholar] [Crossref]
- . Wash,Wipe,Cover...don’t infectanother!. . 2020. [Google Scholar]
- Birring S, Prudon B, Carr A, Singh S, Morgan L, Pavord I. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax. 2003;58(4):339-43. [Google Scholar]
- French C, Irwin R, Fletcher K, Adams T. Evaluation of a cough-specific quality-of-life questionnaire. Chest. 2002;121(4):1123-31. [Google Scholar]
- Cheriamane D, Mohammed G, Verma B, Kandal I, Hari D, Nian S. Knowledge of Cough Hygiene And Disposal of Sputumin Patients with Pulmonary Tuberculosis. Eur Respir J. 2017;16(2):82-5. [Google Scholar]
- Venkatesh U, Srivastava D, Srivastava A, Tiwari H. Epidemiological profile of multidrug-resistant tuberculosis patients in Gorakhpur Division, Uttar Pradesh, India. J Family Med Prim Care. 2018;7(3):589-95. [Google Scholar]
- Bhattacharyya K, Rama R, Mitra S, Bhattacharyya S, TS, Dasgupta U. Perceptions and practices of sputum positive pulmonary tuberculosis patients regarding their disease and its management. NTI Bull. 2005;41:11-7. [Google Scholar]
- Bhatt G, Vyas S, Trivedi. An epidemiological study of Multi Drug Resistant Tuberculosis cases registered under revised national tuberculosis control programme of Ahmedabad City. Indian J. Tuberc. 2012;59(1):18-27. [Google Scholar]
- Akshaya K, Shewade H, Aslesh O, Nagaraja S, Nirgude A, Singarajipura A. Who has to do it at the end of the day? Programme officials or hospital authorities?” Airborne infection control at drug resistant tuberculosis (DR-TB) centres of Karnataka, India: a mixed-methods study. Antimicrob Resist Infect Control. 2017;6(1). [Google Scholar] [Crossref]
- Turner R. Cough in pulmonary tuberculosis:Existing knowledge and general insights. Pulm Pharmacol Ther. 2019;55:89-94. [Google Scholar] [Crossref]
- . WHO operational handbook on tuberculosis: module 1: prevention: infection prevention and control. . . [Google Scholar]
- . Guidelines for programmatic management of drug resistant tuberculosis in India-2021 :: Ministry of Health and Family Welfare. . 2024. [Google Scholar]
- Sharma R, Yadav R, Sharma M, Saini V, Koushal V. Quality of life of multi drug resistant tuberculosis patients: a study of north India. Acta Med Iran. 2014;52(6):448-53. [Google Scholar]
- EY, Smith J. Quality of life in patients with chronic cough. Ther Adv Respir Dis. 2010;4(1):49-55. [Google Scholar]
- Turner R, Bothamley G, Birring S. P240 Validation of the Leicester Cough Questionnaire in pulmonary tuberculosis. Thorax. 2015;70(Suppl3):197-8. [Google Scholar]
- Khan A, Walley J, Newell J, Imdad N. Tuberculosis in Pakistan: socio-cultural constraints and opportunities in treatment. Soc Sci Med. 2000;50(2):247-54. [Google Scholar]
- LP, Yaman N, Heaney L, Cardwell C, Murtagh E, Ramsey J. Impact of cough across different chronic respiratory diseases: comparison of two cough-specific health-related quality of life questionnaires. Chest. 2008;134(2):295-302. [Google Scholar]
- Kelsall A, Decalmer S, Mcguinness K, Woodcock A, Smith J. Sex differences and predictors of objective cough frequency in chronic cough. Thorax. 2009;64(5):393-8. [Google Scholar]
- French C, Fletcher K, Irwin R. Gender Differences in Health-Related Quality of Life in Patients Complaining of Chronic Cough. Chest. 2004;125(2):482-8. [Google Scholar]
- Field S, Conley D, Thawer A, Leigh R, Cowie L. Chronic Cough Is a Woman’S Issue. Chest. 2009;136(4). [Google Scholar]
- Kavalcikova-Bogdanova N, Buday T, JP, Song W. Chronic Cough as a Female Gender Issue. Adv Exp Med Biol. 2015;905:69-78. [Google Scholar] [Crossref]
- Jiyeon K, Seo W, Kim J, Moon J, Kim D, Kim J. Hyeon-Kyoung, Koo. Sex-related disparities in cough-associated symptoms across different age groups. Ther Adv Respir Dis. 2024;18. [Google Scholar] [Crossref]
- Mawey F, Karimah A, Kusmiati T. Workplace interventions to overcome stigma and depression in patients with Multiple drug-resistant tuberculosis (MDR TB). Bali Med J. 2023;12(2):1353-7. [Google Scholar]
- SK, Elsey H, King R, Baral S, Bhatta B, Newell J. Development of a Patient-Centred, Psychosocial Support Intervention for Multi-Drug-Resistant Tuberculosis (MDR-TB) Care in Nepal. PLoS One. 2017;12(1). [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
SA M, Banu S, Sangolli B, BM R, Hatti SS. Practice of cough etiquette and quality of life among MDR-TB patients at a tertiary care hospital [Internet]. IP Indian J Immunol Respir Med. 2024 [cited 2025 Oct 22];9(4):132-140. Available from: https://doi.org/10.18231/j.ijirm.2024.028
APA
SA, M., Banu, S., Sangolli, B., BM, R., Hatti, S. S. (2024). Practice of cough etiquette and quality of life among MDR-TB patients at a tertiary care hospital. IP Indian J Immunol Respir Med, 9(4), 132-140. https://doi.org/10.18231/j.ijirm.2024.028
MLA
SA, Meghana, Banu, Saniya, Sangolli, Basavaraj, BM, Rashmi, Hatti, Shubham S. "Practice of cough etiquette and quality of life among MDR-TB patients at a tertiary care hospital." IP Indian J Immunol Respir Med, vol. 9, no. 4, 2024, pp. 132-140. https://doi.org/10.18231/j.ijirm.2024.028
Chicago
SA, M., Banu, S., Sangolli, B., BM, R., Hatti, S. S.. "Practice of cough etiquette and quality of life among MDR-TB patients at a tertiary care hospital." IP Indian J Immunol Respir Med 9, no. 4 (2024): 132-140. https://doi.org/10.18231/j.ijirm.2024.028
