- Visibility 110 Views
- Downloads 17 Downloads
- Permissions
- DOI 10.18231/j.ijirm.2019.049
-
CrossMark
- Citation
An association between asthma and vitamin D: A prospective study in a tertiary care hospital
- Author Details:
-
Swetha Madas
-
M Hima Bindu *
-
C Mallikarjuna Reddy
Abstract
Introduction: One of the most common chronic diseases is asthma and is related to the hyperresponsiveness of the airways due to prolonged inflammation. The causes for asthma is said to be raised IgE levels and mast cell granulations which are modulated by Vitamin D.
Materials and Methods: 50 patients who were confirmed having asthma were included into the present study. Sputum and blood eosinophil count, IgE levels as well as Vitamin D levels were investigated for all the patients. All the patients were subjected to pre and post bronch odilator spirometry for FEV1 and FVC.
Results: The mean for the Sputum eosinophil count was calculated and was found to be high in the 31(10.13 ± 3.8) Vitamin D deficient group while it was in the normal range (1.97 ± 1.36) among the people with sufficient vitamin D levels. Similar increased levels of eosinophils was seen in the serum and also in the IgE levels. Majority of the patients (14 in number) with deficient Vit D levels had severe asthma (45.2%) and 9 (29%) had moderate asthma. Mild asthma was seen in 6 (19.4%) and intermittent in 2 (6.5%). Atopy was seen in 21 of the patients with deficient Vit D levels and the mean FEV1 % was 61.6 ± 3.7 among the patients with vit D deficient persons and 83.1 ± 6.4 in the vit D sufficient patients
Conclusion: Early detection of the vitamin D levels may help in assessing asthma and its severity in the early stages enabling early and effective treatment, thereby reducing the cost and hospitalization, not to mention the acute exacerbations due to asthma.
Introduction
One of the most common chronic diseases is asthma and is related to the hyperresponsiveness of the airways due to prolonged inflammation. This happens when the airway gets swollen and inflamed resulting in the muscles around the airway to contract cauising the narrowing of the bronchial tubes. This may lead to symptoms such as wheezing, dyspnoea, cough in the mornings, chest tightness etc.[1] Severe asthmatic attacks are many a times life threatening and lead to prompt care and treatment. Such kind of attacks may result in the accelerated loss of functioning of the lung.[2] It has been estimated that around 300 million people worldwide have been affected with asthma in the past few decades and poses an immense burden on health care.[3]
The factors causing asthma are not exactly known and its presentation in the children and in adults is somewhat different. In the asthma patients, the regulation of interleuking happens in the airways and thus increasing in eosinophils, raised IgE levels and mast cell granulations.[4],[5] All these are modulated by Vitamin D as well as its receptors such as macrophages, monocytes and activated t cells and B cells, which suppresses the pro and anti inflammatory cells (interleukins).[6],[7],[8] Vitamin D is fat soluble and is important for the balance of calcium and bone, innante and adaptive immunity as well as to maintain the homeostasis of many organs.[9] Insufficiency of Vitamin D is when the levels of Vit D in blood is less than 30ng/ mL. A value of less than 20ng/mL defined as vitamin D deficiency. Since the levels of vitamin D increase in the presence of sun, high levels of sufficiency is found among the dwellers of the tropical countries. However, now a days a about 30 to 50% of prevalence of deficiency is seen in these countries also.[10],[11] Hence, we attempted to analyze the association between Vitamin D in asthma tic patients.
Materials and Methods
This study was done by the Department of Pulmonology at RVM Institute of Medical Sciences and Research Centre over a period of 18 months from August 2017 to January 2019. 50 patients who were diagnosed with asthma were included into the study. After attaining the clearance from the institutional Ethical Committee, the study was performed. The nature of the study was explained in detail to the patients and their relatives and informed consent was taken from all of them. In case the patients were children, informed consent was taken from their parents / guardians.
Patients who were hospitalised within the past one month or those who have received steroid treatments, bisphosphonates, sulfasalazine, immunosuppresants, phenytoin, omega 3 fatty acids, theophylline or carbazapine were excluded from the study. Those patients having respiratory or systemic diseases as well as those who have taken vitamin D in the past 4 weeks were also excluded from the study.
Demographic details were collected from all the patients and they were all subjected to thorough physical and clinical examination. Sputum was collected from the patients, separated from saliva and stained using Leishman stain for obtaining sputum eosinophil count. Blood was collected and eosinophil count was done in order to get the blood eosinophil count. Serum was separated by centrifugation and IgE was measured with ELISA. Vit D (serum 25- hydroxy - Vit D levels were analysed using chemiluminescence.
All the patients were asked do pre and post bronchodilator spirometry. Forced expiratory volume (FEV1) in litres, forced vital capacity in litres (FVC), FEV1/FVC was done. Increase of FEV1 from baseline was calculated 10-15 minutes after the inhalation of salbutamol (200ug). All the patients were advised not to use bronchodilators for 6 hours and theophylline for the next 24 hours.
All the data were analysed using SPSS software.
Results
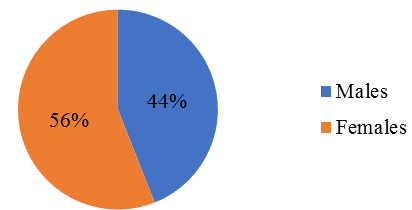
Out of the 50 patients in this study, 22 were males and 23 were females, showing no significant difference in the gender (Fig. 1).
The mean age of the patients in this study was 32.6 years, as some of the patients were children and the elderly. The mean BMI of the 50 patients was 25.1 ± 3.8, while the hips measured 87.2 ± 2.4 cm and waist 75 ± 0.9cm. The mean systolic pressure was 122.2 ± 1.2 mmHg and diastolic 78.3 ± 0.8 mm/Hg ([Table 1]).
| Details | Mean |
| Age | 32.6 ± 1.9 |
| BMI kg/m2 | 25.1 ± 3.8 |
| Waist (cm) | 75 ± 0.9 |
| Hips (cm) | 87.2 ± 2.4 |
| Systolic BP (mm/Hg) | 122.2 ± 1.2 |
| Diastolic BP (mm/Hg) | 78.3 ± 0.8 |
The mean for the Sputum eosinophil count was calculated and was found to be high in the 31(10.13 ± 3.8). Vitamin D deficient group while it was in the normal range (1.97 ± 1.36) among the people with sufficient vitamin D levels (19 patients). The mean values of the serum eosinophil count among the Vitamin D patients was 625.49 ± 44.3, while that in the sufficient group was 221.98 ± 27.24. The IgE levels were 798.31 ± 41.17 units/ml among the patients with deficient vitamin D and 242.21 ± 45.97 among the sufficient persons ([Table 2]).
| Investigations | Vit D levels | Patients (n) | Mean ± SD | p value |
| Sputum Eosinophil count (%) | Deficient Sufficient | 31 19 | 10.13 ± 3.8 1.97 ± 1.36 | ≤ 0.001 |
| Serum eosinophil count | Deficient Sufficient | 31 19 | 625.49 ± 44.3 221.98 ± 27.24 | ≤ 0.001 |
| Serum IgE (units/ml) | Deficient Sufficient | 31 19 | 798.31 ± 41.17 242.21 ± 45.97 | ≤ 0.001 |
Majority of the patients (14 in number) with deficient Vit D levels had severe asthma (45.2%) and 9(29%) had moderate asthma. Mild asthma was seen in 6(19.4%) and intermittent in 2(6.5%). Atopy was seen in 2 1 of the patients with deficient Vit D levels and the mean FEV1 % was 61.6 ± 3.7 in the vit D deficient persons and 83.1 ± 6.4 in the vit D sufficient patients Table 3).
| Asthma | Patients with deficient Vit D (n=31) | Patients with sufficient Vit D (n=19) |
| Intermittent | 2(6.5%) | 6(31.6%) |
| Mild | 6(19.4%) | 9(47.4%) |
| Moderate | 9(29%) | 3(15.8%) |
| Severe | 14(45.2%) | 1(5.3%) |
| Atopy | 21(67.7%) | 5(26.3%) |
| FEV1 (mean %) | 61.6 ± 3.7 | 83.1 ± 6.4 |
Discussion
Modernization and urbanization have lead to the deficiency of vitamin D amongst the population of the world as most of the people now prefer to stay indoor rather than outdoors. With the advent of cell phones, the children also have stopped playing games out in the sun, making them more vulnerable to vit D deficiency.[12],[13]
The mode of action of Vitamin D in the protection from asthma is not clearly known. But a few studies have shown that asthma exacerbations and resistance to therapies are some of the problems faced by the clinic i ans, and Vit D plays a major role in this.[14],[15],[16] Vitamin D is said to promote the steroid sensitivity of the body, regulatin g the inflammatory response through the gene expression and cytokine production, thereby acting directly on the airway, It’s deficiency probably switches off the regulatory action.[17],[18]
In the present study, there was a minor preponderance of females over the males. The mean age in this study was around 32 years, as there were very young children and elderly also included. The BMI was in the normal range, as was the hi p and waist ratio and systolic and diastolic blood pressure.
Among the deficient and sufficient patients, a significant difference was found in the eosinophil count of both sputum and blood. A study done by Guru et al also reported a similar result, where there was a significant difference in the number of patients with higher eosinophil count.[19] Similar results were observed in other studies also. Brehm et al, who reported an increased Vitamin D levels and the IgE levels were inversely proportional to each other as well as eosinophil levels, both sputum and peripheral blood.[20]
The serum IgE levels were significantly lower in the Vitmin D sufficient group compared to the deficient group. This was corroborated in a study by Guru et al who also found the IgE levels to be lower in the Vitamin D sufficient group.[19] In another study by Satwani et al, it was reported that IgE could be a good predictor for allergy and the severity of asthma. Borish et al observed that patients with severe asthma had a higher level of IgE than those with mild asthma.[21],[22] This correlation is useful for the clinical therapy of such patients with IgE.
Majority of the patients (14 in number) with deficient Vit D levels had severe asthma (45.2%) and 29% had moderate asthma. Mild asthma was seen in 19.4% and intermittent in 6.5% in our study. Atopy was seen in 67.7% of the patients with deficient Vit D levels and the mean FEV1 % was 61.6 ± 3.7 among the vit D deficient persons and 83.1 ± 6.4 in the vit D sufficient patients. A similar result was observed by Guru et al who reported that the severity of asthma and the vitamin D levels were inversely proportional to each other,[19] as was observed by Shelb et al.[23] However, a New Zealand study on children upto 5 years of age found no association of Vitamin D levels to asthma.[24]
The limitation of our study was our small sample size. Therefore, the relationship between the Vitamin D and asthma need to be further explored.
Conclusion
There seems to be an inversely proportional relation between the Vitamin D status and the severity of asthma. Therefore, early detection of the vitamin D levels could help in assessing the severity of asthma in the early stages and enabling early and effective treatment, thereby reducing the cost and hospitalization, not to mention the acute exacerbations due to asthma.
Source of funding
None.
Conflict of interest
None.
Acknowledgement
None.
References
- Boulet LP, Fitzgerald JM, Levy ML. Asthma guidelines implementation: a guide to the transalation of GNA guidelines into improved care. Eur Respir J. 2012;39:1220-1229. [Google Scholar]
- Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. New Engl J Med. 1998;339(17):1194-200. [Google Scholar]
- Moore WC, Meyers DA, Wenzel SE. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315-323. [Google Scholar]
- Holt PG, Strickland DH. Interaction between innate and adaptice immunity in asthma pathogenesis: new perspectives for the studies on acute exacerbations. J Allergy Clin Immunol. 2010;125:963-972. [Google Scholar]
- Bradding P, Walls AF, Holgate ST. The role of the mast cells in the pathophysiology of asthma. J Allergy Clin Immunol. 2006;117:1277-1284. [Google Scholar]
- Adams JS, Hewison M. Unexpected actions of Vitamin D: New perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab. 2008;4:80-90. [Google Scholar]
- Damera G, Fogle HW, Lim P, Goncharova EA, Zhao H, Banerjee A. Vitamin D inhibits growth of human airway smooth muscle cells through growth factor-induced phosphorylation of retinoblastoma protein and checkpoint kinase 1. Br J Pharmacol. 2009;158:1429-1441. [Google Scholar]
- Raby BA, Lazarus R, Silverman EK, Lake S, Lange C, Wjst M. Association of Vitamin D receptor gene polymorphisms with childhood and adult asthma. Am J Respir Crit Care Med. 2004;170:1057-1065. [Google Scholar]
- Holick MF. Medical progress: vitamin D deficiency. New Engl J Med. 2017;357(3):266-281. [Google Scholar]
- Glendenning P. Vitamin D deficiency and multicultural Australia. Med J Aus. 2002;176(5):242-243. [Google Scholar]
- Sachan A, Gupta R, Das V, Agarwal A, Awasthi PK, Bhatia V. High prevalence of vitamin D deficiency among pregnant women and their newborns in northern India. Am J Clin Nutr. 2005;81(5):1060-1064. [Google Scholar]
- Kumar J, Muntner P, Kaskel FJ, Hailpern SM, Melamed ML. Prevalence and associations of 25-hydroxyvitamin D deficiency in US children: NHANES. Pediatr. 2001;124(3):362-370. [Google Scholar]
- Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol. 2010;10(4):482-496. [Google Scholar]
- Devereux G, Wilson A, Avenell A, Mcneill G, Fraser WD. A case-control study of vitamin D status and asthma in adults. Allergy. 2010;65(5):666-667. [Google Scholar]
- Urashima M, Segawa T, Okazaki M. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91:1255-1260. [Google Scholar]
- Majak P, Olszowiec-Chlebna -, Mg -, Smejda K. Vitamin D supplementation in children may prevent asthma exacerbation triggered by acute respiratory infection. J Allergy Clin Immunol. 2011;127:1294-1296. [Google Scholar]
- Karatekin G, Kaya A, Saliholu O, Balci H, Nuholu A. Association of subclinical vitamin D deficiency in newborns with acute lower respiratory infection and their mothers. Eur J Clin Nutr. 2009;63. [Google Scholar]
- Ginde AA, Mansbach JM, Camargo CA. Vitamin D, respiratory infections, and asthma. Curr Allergy Asthma Rep. 2009;9:81-87. [Google Scholar]
- Guru H, Shah S, Rasool R, Qadri Q, Guru FR. Correlation between Asthma Severity and Serum Vitamin D Levels: Experience from a Tertiary Care Centre in North India. J Biomedical Sci. 2018;7(3). [Google Scholar]
- Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC. Childhood Asthma Management Program Research Group. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126:52-58. [Google Scholar]
- Satwani H, Rehman A, Ashraf S, Hassan A. Is serum total IgE levels a good predictor of allergies in children?. J Pak Med Assoc. 2009;59:698-702. [Google Scholar]
- Borish L, Chipps B, Deniz Y, Gujrathi S, Zheng B. Total serum IgE levels in a large cohort of patients with severe or difficult to treat asthma. Ann Allergy Asthma Immunol. 2005;95:247-253. [Google Scholar]
- Shebl R, Shehata SM, Elgabry M, Al A. Vitamin D and phenotypes of bronchial asthma. Egypt J Chest Dis Tuberc. 2013;62:201-205. [Google Scholar]
- Sandhu MS, Casale TB. The role of vitamin D in asthma. Ann Allergy Asthma Immunol. 2010;105:191-199. [Google Scholar]
How to Cite This Article
Vancouver
Madas S, Bindu MH, Reddy CM. An association between asthma and vitamin D: A prospective study in a tertiary care hospital [Internet]. IP Indian J Immunol Respir Med. 2019 [cited 2025 Oct 09];4(4):214-217. Available from: https://doi.org/10.18231/j.ijirm.2019.049
APA
Madas, S., Bindu, M. H., Reddy, C. M. (2019). An association between asthma and vitamin D: A prospective study in a tertiary care hospital. IP Indian J Immunol Respir Med, 4(4), 214-217. https://doi.org/10.18231/j.ijirm.2019.049
MLA
Madas, Swetha, Bindu, M Hima, Reddy, C Mallikarjuna. "An association between asthma and vitamin D: A prospective study in a tertiary care hospital." IP Indian J Immunol Respir Med, vol. 4, no. 4, 2019, pp. 214-217. https://doi.org/10.18231/j.ijirm.2019.049
Chicago
Madas, S., Bindu, M. H., Reddy, C. M.. "An association between asthma and vitamin D: A prospective study in a tertiary care hospital." IP Indian J Immunol Respir Med 4, no. 4 (2019): 214-217. https://doi.org/10.18231/j.ijirm.2019.049
